Judith McKay Sides Nigeria 2 (1961-1963)
Judith McKay Sides Nigeria 2 (1961-1963)
Introduction by David Strain gleaned from an email from Judith
Judith McKay (Sides) was a member of Nigeria II, teaching anatomy and zoology from 1961-1963 at the University of Nigeria, Nsukka. She went straight from Nsukka to Tufts Medical School. Between her 3rd and 4th years she obtained a Smith, Kline, French foreign fellowship to work three months at Holy Rosary Hospital in Emekuku, Owerri, Eastern Nigeria, assisting Sister Doctor Mary Macarten of Killeshandra, Ireland.
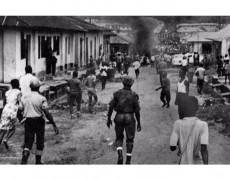
Troubles were brewing when she went to Emekuku in September 1966, though not locally. Most of her time was spent in the wards and in the operating theater, assisting with surgery and the frequent complicated obstetrical emergencies, of which she kept short case histories in a journal. She remembers that the hospital began receiving various trauma cases among Ibos returning hurriedly from the North. Following are two pages detailing four such typical cases: gunshot wounds, machete slash, and forearm fractures from warding off blows. Also included is a write-up of her Emekuku adventure, “plus a bonus photo . . . of my wedding to Richard Sides, whom I met on the trip out and married the day after graduation.”
A FELLOWSHIP IN EASTERN NIGERIA By JUDITH McKAY SIDES, M’67

Judith Sides + Sister Mary Macarten, MD 1 |
Saturday’s arrival at Lagos on September 10, 1966, and our layover between planes was marked by the familiar wait-palaver exasperation known as WAWA (West Africa Wins Again). My one miscalculation was that September would be the onset of the dry season rather than the end of the still soaking rainy season. Two angels in white fetched me damp from the runway at Port Harcourt. Vitalis chauffeured the Peugeot eighty swervy miles north to the compound of the Holy Rosary Hospital at Emekuku (meaning, a very big man), near Owerri in Eastern Nigeria. That evening I met my sponsor and friend, Sr. Mary Macarten, M.D., at the convent for a supper of eggs and British sausages. This was followed by a quick tour of the grounds of the three hundred-bed general mission hospital of which she is the medical superintendent.
HOSPITAL AND STAFF
Holy Rosary Hospital serves about half a million lbo people. Fourteen Irish Catholic nuns, three of them physicians, others nursing and midwifery tutors, technical supervisors, teachers and administrators, together run the hospital, a nurses’ training program for ninety students, and a secondary school in the village. Additional staff includes a talented Spanish surgeon and various Nigerian, Irish, Canadian and American nurses and technicians, secretaries and maintenance engineers on work contracts or volunteer terms of a few months to a few years. I was to be the ten-week all-purpose intern on the premises, and the privileged student of everybody and everything.
On my bookshelf, alongside the standard British texts on surgery, medicine, tropical disease, obstetrics and gynecology, and Doctor at Large, lay a few copies of the Nigerian medical students’ magazine “Dokita,” which I read straightaway. That night’s emergency was an eclamptic woman who had delivered her baby in the bush but chewed her tongue so badly that relatives brought her to the hospital for suturing it back together, a job requiring the surgeon one and a half hours. Sunday was a generally quiet day, characterized by churchbells clanging, swarms of visitors, hilarious checkergames of the domestic help, and siesta terminated by a ruptured ectopic pregnancy coming to the operating theatre.
INTERESTING CASES
I began as first assistant for all surgery, which meant being in the theatre from 7:30 to 4:00 most weekdays. Thursday was hernia day, bread and butter for the hospital at five guineas (c. $15) per operation. We had two basic sets of surgical instruments, so that always one set was in the autoclave while the other was in use. Inguinal, umbilical, epigastric herniae were repaired in fifteen to twenty minutes, allowing me plenty of practice suturing skins and initiating spinals while the surgeon wrote operative notes and orders, rescrubbed and regowned. Theatre sister, Irish, Betty Gaffney, did a splendid job of keeping things running.
 
Nursing, Laboratory, and Secrtarial Staf 1 |
We had an amazing variety of cases on other days well utilizing Dr. Enrico Vaello’s gift and nerve. Take the nephrolithotomy. A young man had come in with recurrent pain in a spot made quite visible by a dibia’s treatments. Native medicine had eaten away an area of skin from his left upper quadrant. Exactly beneath it, intravenous pyelogram revealed a thumb-sized calculus in the left renal pelvis. Under a general anesthetic administered by Dr. Morris, (Sr. M. Macarten), we removed the small staghorn through a posterior approach to the upper pole of the kidney. Patients express interest in their own surgical specimens and usually see them. This chap carried his lucky stone away with him.
One day we did a hemimandiblectomy for a rare adamantinoma. Mr. Nwoke suffered pain and progressive swelling and distortion of his right lower jaw for three years, with dropping out of that row of teeth. X-ray showed a bubbly-looking, tumour-destroyed bone. With three pints of blood on tap, the patient was anesthetized, paralyzed and breathed mechanically through a nasal endotracheal tube. His jawbone was separated at the symphysis and just distal to the right temporomandibular joint with a Gigli saw and was removed. A similarly shaped bone graft taken from his right iliac crest was wired into place. Two days later this good patient was feeding through a nasogastric tube, and within a week swallowing liquids and walking about. His X-ray at three weeks showed no necrosis of the grafted bone. There was a hopeful suggestion of callus formation.
An emaciated old woman admitted for rectal bleeding and anemia revealed a large friable tumour on digital examination. Being sure it was a malignancy and reluctant to cause another hemorrhage, we nevertheless biopsied the lesion. We gave her two pints of blood and sent her home as incurable, though feeling stronger. Six weeks later the pathology report returned from Ibadan – amoebioma. Of course, the poor woman was nowhere to be found. (N. B. Patients near death are preferably taken home before the event because taxi fares quadruple for a dead person and furthermore, the customary mourning clamour disrupts the entire ward.)
At the end of the second week happened a case which each of us in medicine long remembers. Strolling past the female ward after an evening round, I watched a taxi arrive from Enugu, a hundred miles distant. Out tumbled a family very much upset by the sickness of one of its members, a wife. Victoria had gone perfectly well to market that morning, returned about six p.m., and shortly afterward developed the textbook picture of tetany. She showed classical carpopedal spasms and facial twitching, was frightened and hysterical with rapid breathing and nearly unbearable pain.
The nurses could scarcely handle the patient as they endeavored to take her admission temperature, pulse and respirations and dress her in a hospital gown. The spasm worsened with tightening of the blood pressure cuff. The husband alternately pleaded, “Vicky! Vicky!” and tried to give a history. The significant bit was that this had happened twice before, both years in September, and she had been cured by injection, the nature of which they didn’t know. I could only chant to myself, “Tetany means hypocalcemia and that means need for some calcium.” I phoned the doctor on call for advice about a dosage, gave her calcium gluconate intravenously in the less severely contracted left arm, and added intramuscular phenobarbital to help her calm down and go to sleep. A blood calcium level was regrettably unobtainable.
Early the next morning Victoria greeted me with a gratifyingly limp handshake and a smile, complaining of pain in her right hand and requesting a second injection for her right arm! Two days later she insisted on going home. She departed with only a small supply of calcium tablets and admonishments to try to drink milk and to eat liver every week in order to keep that special substance from getting too little into her blood. Like most patients, she would be virtually lost to followup, and she left intriguing questions behind her. Did she have rickets? She had appeared relatively well nourished. Was it a seasonal dietary deficiency? There was no scar on her thyroid region. Had an initial hysteria brought on a hyperventilation alkalosis? Such are the exigencies of practicing symptomatic rather than academic medicine!
FILMING
The highlight of my stay was the visit of the three American photographers from a television station in the Midwest. Not that the personnel hadn’t seen sawed-off blue jeans already, for the Peace Corps is round about. The excitement was generated by all those bright lights and big cameras. Preening was universal, as it became known that everyone was a potential target.
We began the filming with some rounds in the female medical ward and found all sixty patients sitting up freshly combed and shining in their beds, with nary a wrinkle showing in a single sheet.
 Student nurses’ dormitory + classrooms 1 Student nurses’ dormitory + classrooms 1 |
In the operating theatre there was momentary consternation. With cameras rolling and the sister doctor’s scalpel making the first incision, a simultaneous leap and squawk announced that for some fathomless reason the patient’s spinal anesthetic had not taken properly! We proceeded using general anesthesia. Obligingly the suspected uterine fibroid turned out to be a spectacular ovarian cyst. Her delicate feminine fingers dissected the grapefruit-sized sac intact, preserving precious ovarian tissue. They were filming a nice strip of us admiring the cyst when that slippery prize popped out of my hands and headed floorward. The playback of that side-splitting tape sounded like an escapade in a scrap metal shoppe.
Short sequences were shot in most of the laboratories on the compound. In haematology, technicians were making sickle cell preparations and scrutinizing slides for filaria and malarial parasites. Supervisor, American lay missionary R. Rawlings displayed the blood bank refrigerator. Pints are collected as needed for a specific patient from that patient’s male relatives (females’ blood counts are generally too low or borderline). She was proud of a bumper bonus five usable units obtained on a recent expedition to the local prison.
In bacteriology, Sr. M. Francis Therese exhibited positive tuberculin cultures and an agar plate growing pure N. gonococcus. Stools also are cultured, and examined for the ubiquitous Ascaris and hookworm eggs. In the modern X-ray department, Sr. M. Brenda was demonstrating techniques to her trainees. As well as routine plates, she does special studies including IVP’s, GI series, hysterosalpingograms and chest fluoroscopies. The pharmacy was run smoothly under Irish chemist, Aideen Coleman. Her dozen young helpers, in red frocks, fill the daily request slips brought for each patient in a ward basket and entered in a central register.
Sr. Marie Therese, the quicksilver secretary-treasurer, escorted us through the premature baby unit, newly constructed and just awaiting the wherewithal to furnish it. The gift of a preemie incubator is en route froma Canadian physician who spent two years at Emekuku. Other expansions recommended by the boards of accreditation for nursing and doctor-training programs include a modern and better-equipped operating theatre with adjoining surgical wards. That project is still a dream. Gigantic bills and chronic debts must first somehow be paid.
 Encouraging a Small Outpatient 1 Encouraging a Small Outpatient 1 |
OUTPATIENT CLINIC
The most harmonious institution on the compound is the outpatient clinic. Sr. Dr. Mary Luke (Dr. O’Sullivan), an elderly, serene and graceful woman, has conducted it for many years. She sees as many as 150 patients daily. Patients pay a shilling to receive their own clinic cards, line up outside the door, and enter singly as a bell rings. A competent nurse-interpreter elicits the chief complaint from the patient. The sister doctor deftly examines him, asks and answers further questions, and enters the patient’s number, diagnosis and disposition in a ledger. She may advise admission and send the patient to a ward, or baptize a deathly ill child whose parent refuses to admit it. Otherwise she writes orders on the outpatient card, which he carries through the opposite door as the bell rings. He may be directed to a laboratory, where he awaits the results of his tests and returns with them to the doctor. He may go directly to the cash office and thence to the rooms prescribed: Sterile Dressings, Medicines, Injections.
The injection room is a real beehive. Student nurses tend honeycombs of ampoules. Outpatients swarm in bringing their pink cards and line up on benches. One by one they come forward and bare their buttocks. A. nurse eyes the card, selects the correct syringe (used repeatedly for the same drug) from the bank of labeled compartments, draws up the medication, attaches a sterile needle, marks a cross with methylated spirit, and stings him in the upper outer quadrant.
STUDENT NURSE
The student nurse at Holy Rosary Hospital takes pride in her appearance, wearing immaculate starched white uniform, neat head turban and shuffly thongs. The colour of her nametag and sash denotes her degree of seniority. She comes from junior high school, earns her N.R.H. (Nigerian Registered Nurse) in three years, then takes a year of midwifery and becomes a staff nurse. An enjoyable assignment of mine was to lecture the classes in medicine on Wednesday evenings. In return, the nursing matron lent me a second year student, pretty Mary Chigbu, to act handily as my nurse-interpreter. On our endless rounds I shared with hardworking Mary her fascination for medicine and taught her some principles of physical diagnosis.
CHIEF OBI
 Midwives at the bush maternity clinic 1 Midwives at the bush maternity clinic 1 |
When the matron, Sr. M. Aquin, took the photographers and me to call upon Chief Obi of Emekuku Village, Nurse Mary accompanied us. Her sister is one of the respected old chief’s wives, each of whom lives with her children in one of a number of huts surrounding his imposing zinc-roofed dilapidated two-story frame house. Our errand was to persuade the chief to use his influence to discourage the noisy bread and fruit hawkers from their ensconcement at the hospital gate. He consented and dispatched his eldest son, a judiciate, in a car to shoo them away. Then Chief Obi offered us White Horse whiskey mixed with orange pop. We chatted about the current high costs of living and hospitalizations, recalling the old days when the chief’s father had donated the land for the building of the original mission in 1929. He disappeared and reappeared in colorful agbada with his full regalia, including a mug of Star beer made in Nigeria, and delightedly posed for the cameras.
PARISH CHURCH AND WEE SCHOOL GIRLS
An unforgettable occasion stemmed from my having attended service in the parish church one rainy Sunday. Being a Protestant and rather lost during the Mass, I remained after the congregation left between two showers, hoping to collect my thoughts from the past week and my wits for the next. As the downpour continued a small Ibo girl’s face peeked under my elbow and piped, “Sister, may I know whether I shall bring an umbrella to take you home?” In a trice there were six and then twenty wee schoolgirls around us. We talked about families and nurses and bananas and what peanut butter and snow are, and how the nursing sister counts a patient’s pulse to tell how well he is. I taught them to feel their own pulses and heartbeats, which they all did giggling. Then I discovered that only the two who were conversing spoke English, the others not having understood my words. They laughed uproariously at fragments of Ibo language attempted by the onyeacha(meaning, “peeled one”). Inquisitive like puppy paws or tongues, their young hands brushed white arms and light hair.
EMEKUKU VILLAGE
That afternoon the photographers took a ramble through the Emekuku village market, and we encountered my little friend, Benedict Ejiogu, among the children. She remembered and related everything I had said to her that day, and led us to her home. Her mother, Mrs. Katherine, a teacher at the Holy Rosary School, welcomed us warmly and served refreshments. Several of her sons and daughters were summoned to greet us. She asked ten year old Benedict and eight year old Faith to entertain us with recitations, singing and Ibo dancing. Readily and gleefully they displayed their native rhythms. Completely undaunted by the presence of microphone and tape recorder, they astounded us by rendering polished deliveries of long poems by John D. Rockefeller and G. K. Chesterton!
OBS-GYN
Sr. Dr. Calasanctius, (Dr. Tyndall) a board certified specialist in obstetrics and gynecology is a petite woman of indefatigable energy and Irish wit. She draws patients from throughout eastern Nigeria. The weekly antenatal clinic, a longstanding institution regarded as the social gathering of “the day after Sunday,” regularly musters three hundred expectant mothers. Outside, student nurses record brief maternal histories and complaints, serial weights and blood pressures. In six parallel couch cubicles, overseen by two tutors, six pupil midwives record fundal heights, palpate fetal parts and positions and listen for fetal heartsounds. Tablets of antimalarials, antiworms, iron and folic acid are dispensed. All questionable cases are seen by the sister doctor. She may confirm twins, do an external cephalic version of a breech, advise a patient to be admitted for toxemia of pregnancy or a medical illness to the sick prenatal ward, or urge one to go straight to the maternity ward for imminent labour and delivery.
 Expectant mothers a maternity clinic 1 Expectant mothers a maternity clinic 1 |
Postmaturity and its complications are among the stubbornest obstetrical problems in eastern Nigeria. Occasionally the doctor is driven to a morbid device of showing the waiting women a macerated fetus or otherwise dead baby which would have been alive and sucking today but for the folly of its mother’s refusal to come to the hospital before it was too late. This is difficult to understand in a culture where a wife’s goal is to bring forth as many live babies as possible. A partial explanation is the fierce social prejudice against caesarean section and the censure, ridicule or ostracism accorded the woman who cannot deliver her child by the normal vaginal route.
One compromise solution is in the operation of symphysiotomy, called by the women “the little cut” as opposed to “the big cut.” Through a two inch pubic incision the cartilage is divided, gaining perhaps another half inch. Often it relieves the dystocia enough to allow a successful delivery by vacuum extraction with a large episiotomy. This is of course not optimum for the baby, but does present two advantages. First, some enlargement of the birth canal may be permanent, even though the fibrous regrowth is as firm as the original symphysis. Second, the woman who has undergone one “big cut” in the hospital may be loathe to return, and her subsequent delivery in the bush will only be attended by the greater danger of a scar on her uterus.
This is not to say the sister doctors don’t perform several ceasareans each week. Of the twenty or more at which I assisted, one brought us a marvelous spectacle. The indication for operative delivery was a huge prolapsed and strangulated cervix, impossible to dilate though the woman was at term. At a sign of beginning labour the section was done, and foot first came a small surprise twin boy. The other sac remained and came out entire, like a translucent swimming ball with the second twin bouncing and somersaulting inside it. The placenta resembled a large flowery red tam o’shanter on the side of a head. We were so delighted to behold that miraculous globe, showing it to the awestruck mother and calling others to run and see, that we nearly forgot to rupture the wondrous membrane and take the little tyke out! Folklore says a child born so in a lucky “caul” will be a sailor.
Gynae clinic on Saturdays brought an array of women distressed by problems of infertility. Some were years postmenopausal, some newly wed, some still nursing a baby, others barren after 10 years of marriage. Doing 60 consecutive vaginal exams in one morning did teach me the feel of a cervix of any description. Here were collected cases to be done on gynae surgery day: diagnostic D & C’s, laparotomies for lysis of adhesions and plastic repairs of tubes, prolapses and vesicovaginal fistulae.

Listening to a patient with a fetalscope 1 |
All normal deliveries were done by the pupil midwives, who accomplished them quickly with so little fuss that for a time my impression persisted that the labour ward saw a preponderance of abnormal and complicated cases. I was on call to sew all episiotomies, which the nurses saved in batches of two or three to be done at some convenient break. It was one of the few ways in which I actually could lighten the sister doctor’s loads. I relished the practice in suturing techniques, and the nurses amiably noticed my progress from fumbling forty-five minute ordeal to simple fifteen minute task.
To my request of midwife Grace Kanu that she supervise my doing some normal deliveries, her amusingly diffident reply was, “Certainly, Doctor.” As a multipara climbed onto the table, I began to scrub. Before the three minutes were up. Nurse Grace’s indelible voice summoned me: “Doctor, stop scrubbing!” I sped to the table barehanded to deliver that speedy lady’s female baby. Having removed the cord from around her neck I gladly watched her tiny blue face turn pink, look startled, and squall. The placenta too showed an interesting variation known as battledore.
My first weeks were spent in giddy enjoyment of seeing and doing and soaking up everything new and different. There was the intoxication of my first surgical solos: lipoma of the scalp, leg laceration, scrotal cyst, buttock abscess, abdominal paracentesis. I cased the entire hospital from after surgery till late evening, and asked to be fetched in the night for the labour room dramas.
MEDICAL WARDS
During the second half of my stay, the whirling dervish settled into the medical wards. I started learning the day-to-day looks of malnutrition, anemias, parasitism, tuberculosis, hepatitis, pneumonias, peptic ulcer, kidney disease, congestive heart failure, asthma, diabetes, “head pressure”, “waist pains”, and “heat all over the body”. There grew a keen admiration for the acumen and gumption of nursing sister Nova Scotian M. Kavanaugh on the pediatric ward, where children were brought in with cerebral malaria, sickle cell crisis, meningitis, tetanus, measles, pneumonia, kwashiorkor, amoebic dysentery, gastroenteritis and dehydration.
I made myself useful by examining all medical patients on admission. During the final weeks, Dr. Morris was able to entrust to me the morning medical rounds in the male, female and children’s wards. Though innumerable administrative tasks and emergencies hinder her ideal, she believes each patient should be visited, spoken with and appraised daily by his physician. A woman of unbelievable stamina, she works with incisive directness and efficient speed, yet never hurries a patient. At the end of the longest day, she still manages to convey the feeling that she has all the time in the world to talk things over. I missed rounding with her, since I learned from her every examination, question, and esteemed comment.
CONCLUSION
I began practicing what I had absorbed. I came to trust my own stethoscope and ears, eyes and fingers. Those most essential of diagnostic aids do tend to be underrated and overruled in the contention of our own appliance-centered and touch-me-not culture.
What I sincerely hope may have rubbed off onto me is a bit of that quality most genuinely embodied by Sr. Mary Macarten herself: charity. I shall always be grateful for my affiliation with her. May I express an abundant appreciation to both Smith, Kline & French and the American Association of Medical Colleges for providing the springboard to a most wonderful journey!
EDITORIAL COMMENT (in the Tufts Medical Alumni Bulletin)

Wedding Reception, June 10, 1967 a |
Dr. Judith McKay Sides, M’67, received a Smith, Kline & French Foreign Fellowship which she spent from September 10 to November 20, 1966 in Emekuku, Eastern Nigeria. She selected Emekuku because she had been a Peace Corps Volunteer teaching zoology at the University of Nigeria, Nsukka, E. Nigeria, in 1961-63, and had heard at that time of Sister Mary Macarten, M.D. and her work.
Dr. Sides met her husband, Richard St. George Sides, in London in August, 1966 while she was taking a month of neurology at St. Mary’s Hospital, Paddington, en route to the fellowship in Nigeria. Mr. Sides is an honors graduate in history from Trinity College, Dublin. He did graduate study at Oxford and was a District Officer in the former Kenya Administration. At present he is an executive in Ford U. K. Tractor Division.
They were married on June 10, 1967 at her home in North Carolina. They honeymooned in Ireland and are now at home in Elmsleigh, 9 Hillside Road, Billericay, Essex, England. Dr. Sides plans to take the Conjoint Boards in Medicine and Surgery in December. These are the qualifying exams required of all new medical school graduates before beginning internships in England.
Here are two journal pages detailing four typical trauma cases among Ibos returning hurriedly from the North: gunshot wounds, machete slash, and forearm fractures from warding off blows.

http://www.friendsofnigeria.org/StoriesNPictures/Yellow%20Sun/YellowSun-Sides-Corrected.htm



